De Quervain's Tenosynovitis
De Quervain's Tenosynovitis - Information Sheet
2015 PDF 95.8 KB
What is de Quervain’s tenosynovitis, also known as de Quervain’s syndrome?
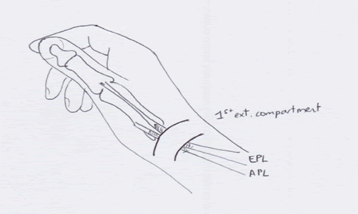
There are two tendons that extend the thumb: Abductor pollicis longus (APL) and Extensor pollicis longus (EPL). As these tendons travel from the forearm into the hand, they run through a tight tunnel. The tunnel is part of the extensor retinaculum, a broad ligament that binds the tendons down against the forearm, and allows the tendons to work efficiently. The tunnel and the tendon are covered with a layer of tissue called tenosynovium to help the tendons glide as they move through the narrow tunnel.
In De Quervain’s tenosynovitis, inflammation of the tenosynovium narrows the tunnel. This means that the two tendons do not move easily but graunch and grind their way through, which is very painful.
Why does it occur?
There are a number of causes. It can be a result of age related degeneration, when either the tendon or the sheath swells and thus restricts easy movement. Another cause of this condition is local trauma for example a blow to the thumb side of the wrist. Recent unusual overuse, especially repetitive use of the hand and wrist, for example, gardening and hammering can also cause de Quervain’s syndrome.
Your symptoms may include:
- Pain near the base of your thumb
- Swelling near the base of the thumb and up onto the thumb side of the lower forearm
- Pain on moving the thumb, making a fist, grasping or holding objects
- A snapping or catching feeling when you move your thumb
- A positive Finkelstein’s test: The pain gets worse when you grasp your thumb within the palm, and you bend your wrist to the side.
Which options do I have to treat De Quervain’s tenosynovitis?
Conservative (non-surgical) treatment
We will talk about your treatment options, including their risks and side effects, during our initial consultation. I often recommend that you try non-surgical treatment first, as non-surgical measures may resolve up to 70% of De Quervain’s symptoms over about 6 weeks.
- Rest
- Anti-inflammatory medication: Diclofenac (Voltaren) or Ibuprofen (Nurofen)
--> Not advised if you are allergic to this medication, have stomach ulcers, asthma or kidney failure.
- Splint: This is used to immobilize your wrist and thumb.
- Steroid injection: Steroids are very helpful in treating the problem. They reduce the inflammation and swelling of the tenosynovium and allow the tendons to glide easily.
--> Side effects of steroid injections: thinning and discolouration of skin around the injected area, development of fine blood vessels (telangiectasia) and infection (redness, swelling, throbbing discomfort). Two injections is the maximum I will administer as side effects become more prevalent with increasing injections.
--> Diabetic patients: Your blood glucose control may be more variable and difficult to control for the next few weeks.
Surgical treatment – De Quervain’s release or 1st extensor compartment release
Surgery is sometimes required for De Quervain’s tenosynovitis, but only after we have tried to relieve your pain with non-surgical treatment.
The operation is performed under local or general anaesthetic. During the procedure, I make a small incision of about 2-3 cm along the thumb side of your forearm, towards the wrist. The tendon sheath is divided and explored. By dividing the sheath, I give your tendons plenty of room to move, preventing pain from forcing the tendons through the swollen tunnel.
As the final part of the procedure, your wound is sutured. I will apply a light dressing and provide you with an information sheet about wound care and exercises.
Your recovery after surgery
You may drive a car at about a week, provided your wrist is comfortable and you are able to control a motor vehicle safely. Your return to work depends on your level of occupation: Office workers may need a few weeks’ leave from work while heavy manual labourers will more likely need about 6 weeks.
Possible complications of De Quervain’s release surgery
Wound complications
Possible problems include swelling, bruising, bleeding, blood collecting under the wound (haematoma), infection and splitting open of the wound (dehiscence).
Scarring
The scar may become a little thickened and red as it heals, but this will settle with time. The scar will be tender, and this will also resolve. Once your wound is healed, tape on the wound for 6 weeks, followed by firm massage with a plain cream or oil will help optimise the scar.
Nerve damage / Neuroma
There are small nerve branches that run in the area of the incision. The nerve can occasionally be damaged during the operation, and this may leave either a numb patch on the back of your thumb, or a small tender point that may need another small operation to excise the tender spot.
Stiffness
Exercises should resolve this. If you do not have a hand therapist, I will recommend one during our follow-up consultation, or you can read more about the hand therapists I refer to frequently.
Complex regional pain syndrome
About 5% of patients have nerves that are very sensitive to surgery and trauma; they develop a very painful, stiff and swollen hand after the operation. The symptoms are out of proportion to the nature of the operation. At the moment, we are not sure why it happens and we cannot predict whom it will happen to. I will monitor you for this after the operation, and the treatment involves special forms of pain relief and physiotherapy. Please read more about Complex regional pain syndrome.
Tendon movement
The division of the sheath that usually binds your tendons down can cause the tendons to move from side to side when you bend your wrist. This may be an odd sensation, but it usually causes no further trouble.
Please read about Complications following hand surgery.
Want to make an Appointment or have an Questions?
You may have some specific questions around procedures, treatments, appointments, timeframes or costs. Contact Dr Rebecca Ayers using the form on the contact page.
Find out more