Breast Reduction and Mastopexy
Breast Reduction - Information sheet
2015 PDF 127 KB
Breast reduction vs. Mastopexy
A breast reduction is when the size of your breasts is reduced. This procedure is usually accompanied by a breast lift.
A mastopexy is a breast lift while the overall size of the breasts remains almost the same.
While the information on this page focuses on breast reduction surgery, most of it is relevant for mastopexy, too. As with all information on my website, please ask me any detailed questions you might have during our consultation.
Is a breast reduction the right procedure for me?
If you have large and heavy breasts, you may experience one or more of the following issues:
- Back, neck and shoulder pain
- Grooves in your shoulder skin from bra straps
- Sweating, rashes and skin infections under your breasts
- Difficulty participating in sport
- Self-consciousness and psychological distress due to the size of your breasts
- Unwelcome and inappropriate comments from others
In a breast reduction, I remove skin, fat and breast tissue to reduce the size of your breast and elevate the position of your nipples.
Pre-operative preparation
For the best results, it is best if your body mass index (BMI) is as close to normal as possible, and you are smoke free. If you have given up smoking, I advise you not to use nicotine replacement therapy for four weeks before and four weeks after your operation.
If you are above the age of 40, it is recommended to have had a mammogram within the last 12 months before the procedure.
What is the technique for breast reduction?
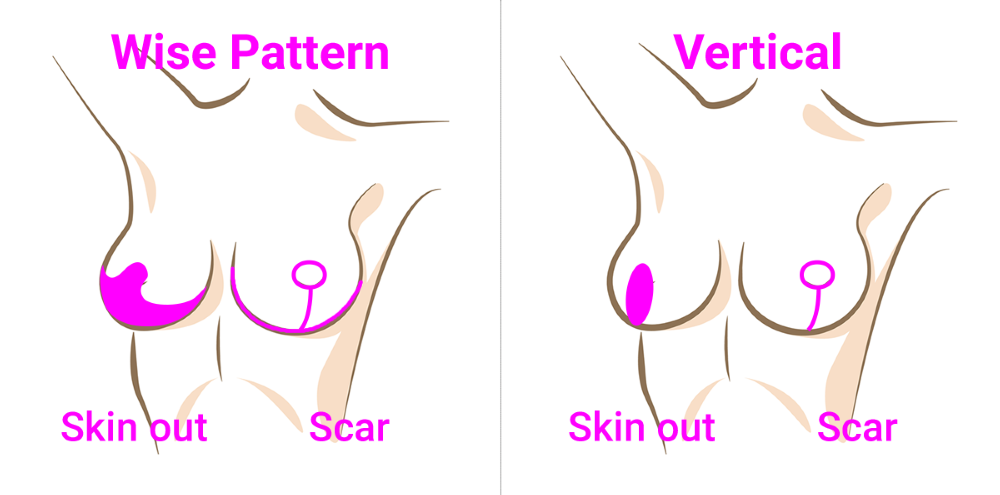
The operation takes between three to four hours and involves reducing the skin and soft tissue of your breast. The scar is usually anchor shaped (a Wise Pattern reduction): extending around the areola, down the front of your breast and underneath the breast. Sometimes, for smaller reductions, the scar underneath the breast may be shorter (a Vertical reduction), but this is less common. The blood supply to the nipple is maintained by the ‘pedicle’ which connects the nipple to your chest wall. Preserving the blood supply to the areola is important for easy healing of the nipple and areola.
Sometimes for very large reductions, so much breast tissue is removed that the nipples must be removed and then replaced as a graft. This may cause delay in healing of the nipple, or partial or total nipple loss.
Sutures are almost always dissolving. After the operation, there will be a drain left in each side.
All the wounds will be taped. I prefer Micropore tape.
Breast reduction: the procedure and your recovery
What should I bring to hospital?
It is important that you bring a few suitable post-operative bras with you. The best are soft, supportive, non-underwire bras like sports or maternity bras. They need to have a cup shape to help support your new breasts. Keep the labels on, so you can return them (un-used!) if they don’t fit. This also helps to give me an idea of the size you would like your breasts to be.
I like you to have some MicroporeTM tape available for after the operation. This tape can be purchased from your local pharmacy.
From 6 weeks after your operation, I will ask you to moisturise the scars. Ask your pharmacist for a plain, hypoallergenic, unscented moisturiser. I don’t recommend a particular brand.
Desired size
I cannot guarantee a particular size, as that depends on the size of your torso and width of your chest. It is important to remember that very small breasts may make your tummy (if you have one!) look larger. Ultimately, I aim to improve your symptoms while creating attractive breasts, with a long-term pleasing shape.
After your breast reduction surgery
It will be painful after the operation, and you will be given oral pain relief. A small injection is given into your tummy to reduce the risk of blood clots developing in your legs and lungs (DVT, PE).
You will be in hospital for 1-2 nights, but you will need help at home with shopping, housework and childcare for at least 2 weeks following the operation. It will be 4-6 weeks before you feel back to your usual self, and you will need to take things easy during this time.
The drains I put in place at the end of the surgery will come out before you leave hospital. There may still be a little ooze from the drain sites for the next few days but it should stop very quickly.
After 48 hours, you can shower briefly. It is fine for fresh water, soap and shampoo to run over the wounds. Avoid bathing in a bath or swimming pool until the wounds are completely healed. After showering, the tapes should be dried carefully by leaving the tapes open to the air or by using a hairdryer on cool (a hairdryer on warm or hot may burn the wounds!). The tapes can stay on for 7-14 days, however if they become loose, tatty or moist then the tape may be changed earlier.
Please wear a good supportive, non-underwire bra all the time (23 of 24 hours a day) for the first 3 months. This is to support the breast tissue as it heals. After that, you may return to wearing a bra as you wish.
You should avoid strenuous activity for at least 6 weeks; be guided by how you feel and be sensible.
When can I start driving again after my surgery?
It is best not to drive for at least 2 weeks following the operation. You may return to driving when it is comfortable to wear a seat belt and you feel confident and comfortable to control a motorcar.
How can I improve the scars?
Keeping the scars taped for 6 weeks is important. After that the scars can be massaged twice daily with a plain, unscented, hypoallergenic moisturising cream. It is very important to avoid any UV exposure for 12 months following the operation; UV exposure can cause the scars to pigment strongly. The scars should fade and flatten over 12 months.
To start with, the scars are fairly small and it is usual for scars to thicken and become red as they heal. If your scars become very red, itchy or thick then please contact me as you could be developing hypertrophic or keloid scarring that may need special silicone dressings or steroid injections.
How will my breast reduction change over time?
Your breasts will still be affected by gravity, weight change and time. They will continue to change shape as you age.
Possible complications
Pain
Pain is usually not severe and can be managed by oral pain relief. It is often worse when you move around and cough. This pain settles with time. If you have tender breasts before the operation then the breast reduction is unlikely to cure this.
Infection
Wound infection can occur after any surgical procedure. A dose of antibiotics is administered at the beginning of the operation and further antibiotics are not routinely given as this leads to antibiotic resistance. The signs of infection are increased redness, discharge from the wound, fevers or feeling unwell (similar to getting the ‘flu). Infection requires more antibiotics and sometimes admission to hospital or an operation to resolve it.
After your surgery, if you feel like you may have an infection, please get in touch with me so I can review your wound and prescribe antibiotics if needed.
Bleeding
Bleeding can be minor or it can lead to a collection of blood (a haematoma) that needs to be drained in theatre. Your wound will be monitored for bleeding while you’re in hospital. If you are concerned about bleeding at any time after your operation, please let me know.
Asymmetry
No two breasts are identical. There may be some asymmetry in size and shape of the breasts and areolas following the operation.
Wound healing problems
Sometimes the wounds take a longer time to heal and may require dressings for some weeks. This is especially true of smokers and women who are overweight.
Partial or total loss of nipples
Breast reduction involves changing the position of the nipples and reduces the blood supply to the nipples. Usually there is sufficient blood to supply the nipples, but occasionally a part or the entire nipple dies. If this happens during your surgery, I will treat it with dressings, and then I will perform nipple reconstruction at a later date.
With a standard pedicled breast reduction, the risk of losing your nipples is low. However if you have a nipple graft then the chance of there being a problem with the healing of your nipples or the loss of your nipples will be high.
Change in nipple sensation
Usually there is decreased or no sensation within the nipples following surgery. This is because the nerves have been cut during the surgery, and this is permanent. Occasionally, the nipples become more sensitive.
Scars
There will be permanent scars following the operation. Hopefully these scars will be fine and pale, but some people have a tendency to poor scarring and their scars can be thickened, itchy and unsightly (hypertrophic or keloid scarring). Occasionally, revision surgery is needed for scars.
Breastfeeding
Breastfeeding ability is usually significantly reduced following a pedicled breast reduction and impossible following a free nipple graft. If breastfeeding is very important to you, you may want to postpone the reduction until after your family is completed.
Fat necrosis
The operation changes the blood supply of the breast and this may lead to part of the fat of the breast dying and causing a small scar, which feels like a lump. All breast lumps must be investigated thoroughly to exclude cancer. Please talk to me during our post-surgery consultation if you feel a lump may be developing in your breast.
Unexpected diagnosis of cancer
The breast tissue that has been removed is sent for analysis and occasionally an unexpected diagnosis of cancer is made. Should this be the case, I will assist you with initiating any treatment that may become necessary.
Want to make an Appointment or have an Questions?
You may have some specific questions around procedures, treatments, appointments, timeframes or costs. Contact Dr Rebecca Ayers using the form on the contact page.
Find out more